I am an Air Force wife. My husband battles persistent depression and suicidal ideation. As many are acutely aware, suicide and depression is at an all-time high among our military men and women, and unfortunately, my husband is not an exception.
I know that he is not alone; he recently completed an eight week partial hospitalization program that was specifically for active duty military. So many people are struggling.
I know that as a spouse, I am not alone, but I have not seen many spouses publicly writing and speaking out about this issue. I get it — it is scary and there could be repercussions on a career, the next move, the recommendation, finances, kids, home stability, and more. If this is you, you are not alone. I am in this battle with you.
Being the wife of anyone who is suicidal is excruciating. There are many components in play and not knowing what I may or may not come home to is unsettling. It takes a toll on me as a person, on my marriage, and on my kids. As such, I believe that spouses are on the front lines of this issue. Servicemen must keep it together all day for co-workers and commanders, but we see how that impacts them. I firmly believe that spouses are the system experts in this fight because we see the facets that the Air Force cannot. It is a hard position to be in.
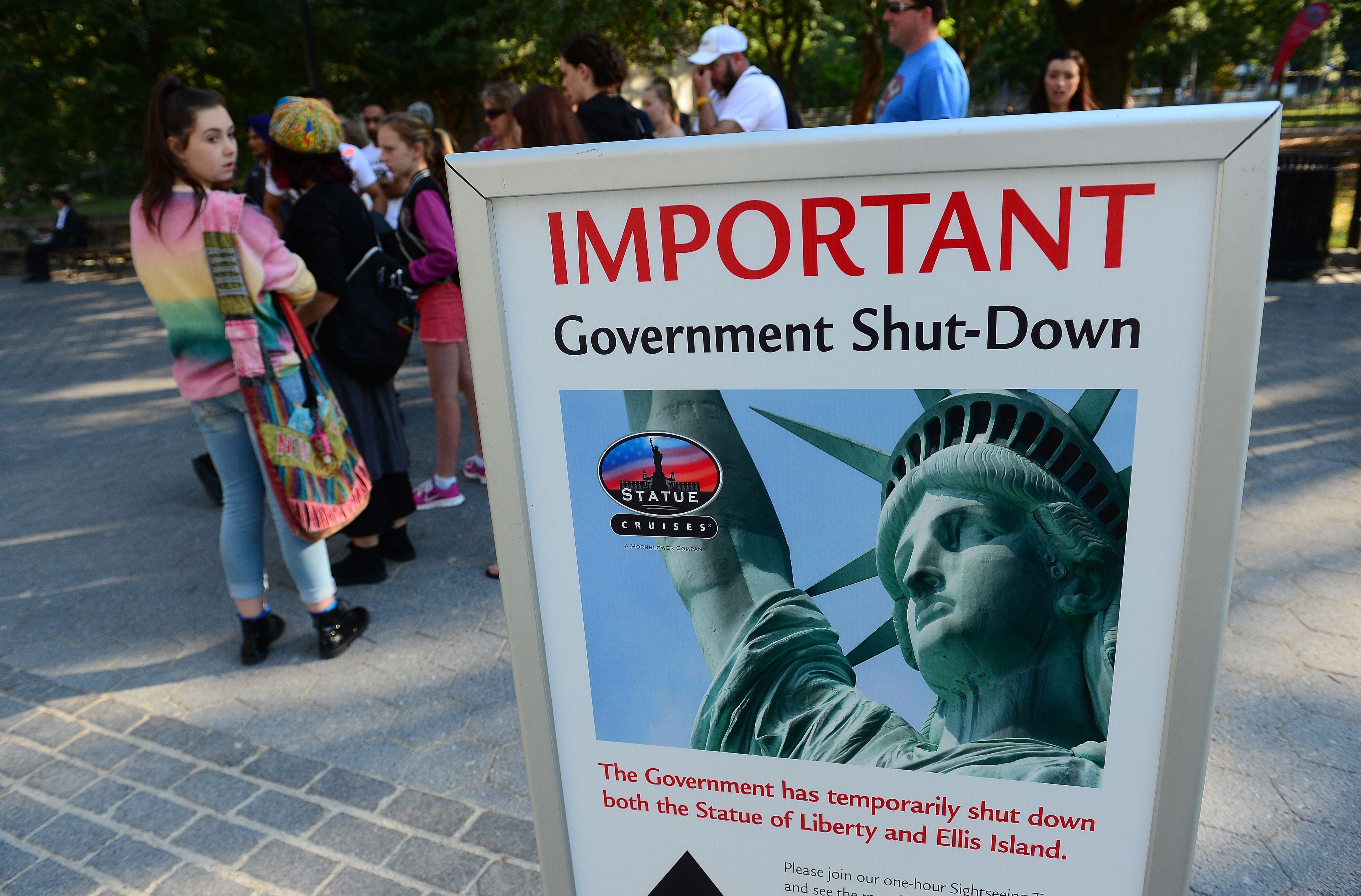
I believe that the problem of depression and suicide in the military is underreported and widely underestimated. It is a problem that no one wants to have and few want anyone else to know that they deal with. There have already been suicides because of the lockdown and shelter-in-place orders. Human contact and relationships are a necessity and when those already struggling have their lifelines and routine shut down, it is a battle to simply stay sane.
I live with someone who struggles very much. He is now on medication to try and cope with unwanted suicidal thoughts and depression; he is one of many. A 2014 article by the Military Times reported that 1 in 6 active duty members are taking psychiatric drugs. That is just the 16.7% who have spoken up and received some form of psychotropic medication. I suspect that there are many more who suffer in silence. If that is you, my heart goes out to you and you are not alone.
Suicide, depression, and mental health concerns are systemic in the armed forces. There are many factors and I do not think that those have been properly vetted and understood. From this spouse’s perspective, the military seems to want to slap a Band-Aid of a program on it and call it fixed. Those Band-Aid programs sent my husband further underground and only coached him on what not to say. The military is a psychologically challenging (but very rewarding) career, yet I think a few changes can help make situations easier for struggling service members.
First, there is a simple solution for providing more continuity to reduce turnover with mental health. My husband had three mental health service providers in a matter of weeks (again, I have heard that he is not alone with this) and his current provider is scheduled to move in the fall. That erodes the therapeutic relationship and when sensitive information is being discussed, trust and stability must be present. I believe extending assignments to a five-year minimum for mental health therapists or homesteading them altogether would help with some of this instability. The system is very fractured and disjointed, and this would potentially allow for some relief. As a bonus, the military saves money on moves.
Second, guaranteeing off-base counseling would demonstrate the military’s commitment to supporting our nation’s elite and give those who feel out of control the ability to choose someone they trust and work with. This small part could provide an enormous impact. Allow for a member to simply request off-base therapy and then be free to see any therapist who takes Tricare with automatic approval. The military will know who is going off base and the service member can see someone they feel comfortable with.
Third, there is a questionnaire that my husband must answer before seeing a provider in mental health. Since he is in the Air Force, I do not know if this is across all branches or Air Force specific. The questionnaire varies every time depending on how a respondent answers questions; it is not standardized, takes 20 or more minutes, and almost all the same questions are asked again in session, creating a frustrating redundancy. I understand that this is to track progress and data points, but the therapist can manually enter the answers and be able to use the questions as a tool or jumping off point and not create such frustration among a community that is already at a breaking point. People who have mustered the courage to seek mental health care do not need any additional roadblocks when trying to see a provider.
As a concerned citizen and wife, I have written Air Force leadership and members of Congress, but I have not received a response from anyone. I want to discuss with someone what is going on from a spouse’s viewpoint. I believe that many spouses see things that members walking through this cannot, and we are experts in our own way regarding this epidemic. We are fighting our own front-line battles with this while also raising children, working, and trying to keep ourselves afloat. Things need to change and I am willing to step up and do something about it.
Aleha Landry lives in Colorado with her husband and four children, and has spent the last decade as a stay-at-home mom. She has a passion for politics and policy, hates to cook (but cooks much due to aforementioned children), and loves to travel. She holds a bachelor’s of business administration from Colorado Christian University. You may reach her at aleha.landry@gmail.com.
Editor’s note: This is an Op-Ed and as such, the opinions expressed are those of the author. If you would like to respond, or have an editorial of your own you would like to submit, please contact Military Times managing editor Howard Altman, haltman@militarytimes.com.